Last September, Erin Bell went to her doctor for a biennial mammogram.
While the Vancouver woman was cancer-free, her doctor recommended a bilateral breast ultrasound — which can be used to detect cancer in women with dense breast tissue, who are at greater risk of developing cancer.
A year after, Bell, 48, got a call from her doctor — not to schedule an appointment, but to inform her that she’d have to go to a private clinic to do so.
“I got a call from my doctor’s office from the reception there saying that the clinic that schedules the bilateral breast ultrasound is not taking any more patients,” Bell told CBC News.
“That’s all she said to me. She said she’s making that phone call to a lot of people and she has no more information. She’s just the bearer of bad news,” she added.
Bell started calling around to find out how much it costs to pay for the test through the private system, and was given a quote of $700 — and potentially even higher south of the border.
The former kindergarten teacher, who is on long-term disability due to suffering from long COVID, says that going through with the test was important for her as early breast cancer detection is known to save lives.
While a bilateral breast ultrasound for those with dense breasts is covered by the Medical Services Plan (MSP), the provincial health insurance program, demand is exceeding supply in B.C.’s Lower Mainland, which only has one clinic that performs the procedure.
A backlog of patients means the only way she’s likely to get an ultrasound is to pay at a private clinic.
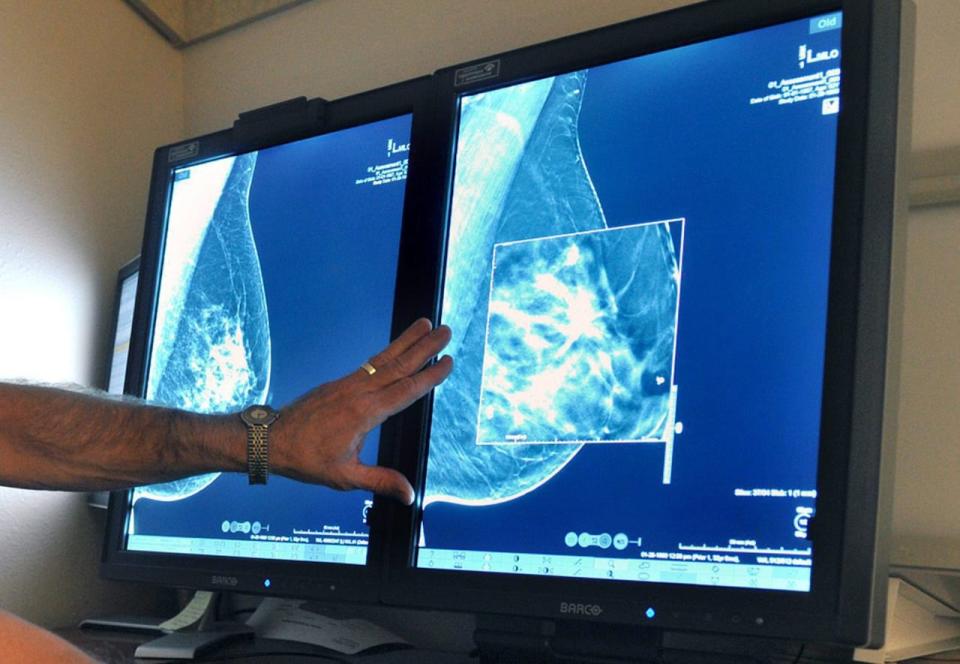
Mammography is the main tool used to detect any potential breast cancer in Canada. (Torin Halsey/The Associated Press)
“I honestly don’t know what to do because I’m on disability, $700 is a lot of money,” Bell said. “We have health coverage. We’re not supposed to have to pay for things.”
A doctor who pushed for women with dense breasts to get extra tests says the province needs to change its fee structure for doctors to allow them to get appropriate compensation for a bilateral breast ultrasound.
Two types of ultrasound
Dr. Paula Gordon, a clinical professor at the University of B.C., does breast radiology and intervention needle biopsies.
She says ultrasound tests can be used for diagnostic purposes — when a lump shows up in a woman’s mammogram — and involves sound waves making a “picture” of the affected area.
A more involved procedure, called the screening breast ultrasound, involves scanning the entire breast, she says.
“In British Columbia, in order to have a screening breast ultrasound, you have to have dense breasts, either Category C or D, and that’s really important,” she said.


Dr. Paula Gordon, a clinical professor at the University of B.C., does breast radiology and intervention needle biopsies. (Submitted by Dense Breasts Canada)
Gordon says that for some time her clinic was performing screening breast ultrasounds for people all across B.C. and even other provinces — and it got to the point where they were fully booked months in advance.
The doctor said her clinic performed 3,000 exams in 2022 alone, a testament to the fact not many clinics perform the procedure.
She adds that MSP did not create a fee specific to the screening breast ultrasound — and instead told her to bill the insurer the same amount that she would have billed for a diagnostic exam.
“The fee for diagnostic [exams] is really not adequate to justify the time that it takes to do a full both-sides screening breast ultrasound,” Gordon said.
Minister says he would look at fees
Health Minister Adrian Dix says B.C. was the first province to provide women their breast density information when they went in for cancer tests.
“We’ve seen an increase in diagnostic screening, breast diagnostic screening in the past year and significantly in terms of numbers that we have to expand out that access,” Dix said.
“And we’re happy to look at issues around fee codes to make sure that doctors have the right incentives.”


Health Minister Adrian Dix says B.C. was the first province to provide women their breast density information when they went in for cancer tests. (Michael McArthur/CBC)
A spokesperson for B.C.’s health ministry said the average time to book a mammography in B.C. is 8½ weeks as of July, and there were nearly 270,000 screening mammograms conducted in the province last year.

